Bone-on-bone knee pain is a debilitating condition caused by the deterioration of articular cartilage in the knee joint, leading to direct contact between bones. This bone friction results in pain, stiffness, and reduced mobility, significantly impacting daily life. Conditions like osteoarthritis or posttraumatic arthritis often contribute to this issue, making it critical to seek early intervention. Addressing this pain early can prevent complications such as bone spurs, joint stiffness, and further cartilage loss. This article dives into the causes, symptoms, diagnostic methods, and treatment options, including ways to manage bone-on-bone knee pain relief effectively.
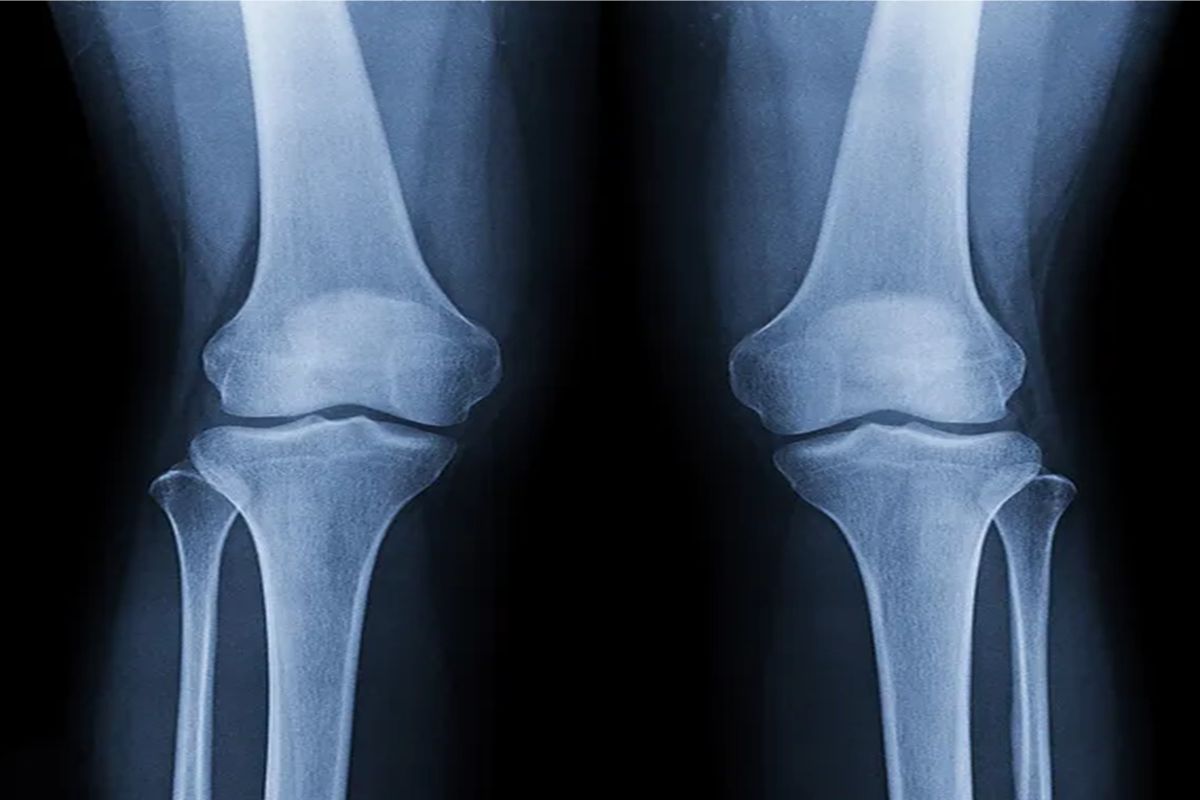
Structure of the Knee
The knee joint is a complex hinge joint composed of the femur (thigh bone), tibia (shin bone), and patella (kneecap). Cartilage cushions these bones, enabling smooth movement and absorbing shock. Supporting structures like ligaments, tendons, and muscles provide stability and mobility. Damage or wear to cartilage disrupts this balance, often leading to bone-on-bone contact and pain. Globally, knee pain affects 10% to 60% of the population, with older adults particularly vulnerable. As the most prevalent joint disease, osteoarthritis significantly contributes to knee pain, making it one of the leading causes of chronic pain and mobility issues worldwide.
What Causes Bone-on-Bone Knee Pain?
Bone-on-bone knee pain can result from various causes, with osteoarthritis being the most common. This condition, characterized by cartilage loss due to aging or joint stress, progresses through multiple knee osteoarthritis stages, accounting for over 80% of the total burden of joint diseases. In the United States alone, approximately 19% of adults aged 45 and older are affected by knee OA, highlighting its significant public health impact. Other causes include injury, such as fractures or ligament tears, which can hasten cartilage degeneration. Rheumatoid arthritis, an autoimmune disorder, damages the articular cartilage and joint linings, leading to synovial membrane inflammation. Obesity also plays a critical role, as excess weight increases pressure on weight-bearing joints, accelerating cartilage wear. Additionally, a genetic predisposition, such as a family history of degenerative joint disease or certain genetic markers, can elevate the risk. Lastly, repetitive physical activity or occupational strain stress contributes to cartilage breakdown over time.
How Does Bone-on-Bone Knee Pain Feel?
Bone-on-bone knee pain presents differently, ranging from a dull, persistent ache to sharp, sudden discomfort during movement. Pain may radiate to nearby areas or remain localized, often indicating uneven cartilage wear. Recognizing these pain patterns helps identify the condition and its severity.
Dull and Achy Pain
A persistent, deep ache in the knee is a hallmark of cartilage loss, often worsening after prolonged activity or at the end of the day. This type of pain is typically associated with the gradual progression of osteoarthritis or other degenerative conditions. It may also be accompanied by stiffness, especially after sitting for long periods or first thing in the morning.
Sharp Pain
Sudden, intense pain during movement, such as when standing up or climbing stairs, often indicates advanced joint damage or the presence of bone spurs. This sharp pain can make weight-bearing activities difficult, impacting mobility. In some cases, it may also signal micro-tears in surrounding tissues or irritation of the synovial membrane.
Radiating Pain
Discomfort may spread to surrounding areas like the thighs or calves, a result of joint misalignment or compensatory movement patterns due to gait problems. This radiating pain can lead to additional stress on other joints and muscles, compounding the discomfort. Over time, it may also affect overall posture and alignment, further exacerbating knee issues.
Localized Pain
Pain confined to one part of the knee, such as the inner or outer side, may signal uneven cartilage function or a degenerative meniscal tear. Localized pain often correlates with specific wear patterns, such as those caused by repetitive stress or prior injuries. Pinpointing the exact area of discomfort helps diagnose the underlying issue and tailor treatment options.
Diagnosing Bone-on-Bone Knee Pain
Diagnosing bone-on-bone knee pain involves evaluating the patient’s medical history, conducting a physical examination, and using imaging techniques like X-rays or MRI scans. These tools help visualize cartilage loss and pinpoint the condition’s cause, guiding effective treatment plans. Many patients benefit from expert assessment and treatment recommendations provided by Austin physical therapy clinics.
Review of Patient’s Medical History
A thorough medical history review helps identify potential causes, such as previous injuries, family history, or conditions like rheumatoid arthritis. This step provides valuable context, helping to differentiate bone-on-bone knee pain from other joint disorders. It also offers insights into lifestyle factors, such as repetitive stress or weight-bearing activities, that may contribute to the condition’s progression.
Physical Examination
Doctors assess joint stiffness, range of motion, and tenderness to determine the severity and location of the pain. Tools like a knee pain location chart are often used to pinpoint affected areas more precisely. Additionally, they may evaluate for signs of joint swelling, muscle weakness, or gait problems to understand the knee’s functional limitations.
Imaging Tests
Imaging tests are crucial in diagnosing bone-on-bone knee pain by providing detailed insights into joint health. X-rays are commonly used to reveal joint space narrowing, bone damage, and the presence of bone spurs, helping to identify the extent of cartilage loss. For a more comprehensive view, Magnetic Resonance Imaging (MRI) offers detailed visualization of articular cartilage, meniscus cartilage, and soft tissues, allowing for a thorough assessment of the joint’s condition. In cases requiring a closer look at bone alignment and structural abnormalities, Computerized Tomography (CT) scans provide cross-sectional images that highlight areas of damage, supporting precise diagnosis and treatment planning.
How to Relieve Bone-on-Bone Knee Pain
Knowing how to relieve bone-on-bone knee pain involves adopting a combination of treatments tailored to the severity of the condition and the patient’s overall health. Relief strategies range from non-invasive approaches, such as physical therapy and medications, to advanced options like injections or surgery. A comprehensive approach can help alleviate discomfort, improve joint function, and enhance overall quality of life.
Non-Invasive Treatments
Non-invasive treatments provide effective relief for bone-on-bone knee pain without surgery. These approaches are a key component of arthritis treatment, focusing on reducing inflammation, improving joint function, and managing pain through therapies and lifestyle modifications. By exploring these options, individuals can enhance their quality of life while delaying or avoiding more invasive procedures.
- Applying Ice Packs: Ice reduces inflammation and numbs pain, offering immediate relief, especially after activity. Applying an ice pack for 15-20 minutes at regular intervals can help control swelling and reduce discomfort. It is particularly beneficial after activities that strain the knee, providing a simple and effective way to manage acute pain.
- Pain Medication: Nonsteroidal anti-inflammatory drugs (NSAIDs), both oral and topical, alleviate pain and swelling. These medications reduce inflammation at the site of joint damage, making movement less painful. Over-the-counter options are often sufficient, but prescription-strength NSAIDs may be recommended for more severe cases.
- Physical Therapy: Targeted programs focus on improving joint function, range of motion, and strength while addressing gait problems. Physical therapy sessions often include exercises tailored to the individual’s condition, promoting better mobility and stability. Therapists may also incorporate techniques such as ultrasound therapy or manual therapy to alleviate pain further.
- Strengthening Exercises: Exercises that target the core and leg muscles improve stability, reducing stress on the knee joint. Strengthening the quadriceps and hamstrings helps absorb shock and support the joint during daily activities. Activities like knee rehabilitation exercises like leg lifts or squats are designed to be gentle yet effective in restoring strength and balance.
Intra-articular Injections
Intra-articular injections provide targeted relief for bone-on-bone knee pain by addressing inflammation, lubrication, and cartilage health. Corticosteroid injections are commonly used to reduce inflammation and alleviate pain effectively. Hyaluronic acid injections (viscosupplementation) improve joint lubrication, making movement smoother and more comfortable. Additionally, regenerative treatments like Platelet-Rich Plasma (PRP) and stem cell injections are designed to enhance cartilage function, offering innovative options for long-term joint health and repair.
Knee Replacement Surgeries
In severe cases, procedures such as partial knee replacement or total knee replacement restore joint function and significantly reduce pain. These surgeries involve replacing the damaged portions of the knee with artificial implants, which can last for many years with proper care. For patients looking to delay surgery, newer approaches like regenerative medicine techniques provide promising alternatives, focusing on improving cartilage function and reducing symptoms through less invasive means. Advances in surgical technology have also shortened recovery periods and improved outcomes, making these procedures safer and more effective.
Lifestyle Changes to Prevent Bone-on-Bone Knee Pain

Adopting healthy lifestyle habits can significantly reduce the risk of developing or worsening bone-on-bone knee pain. Preventive measures focus on minimizing stress on the joints, maintaining overall mobility, and promoting joint health. By making simple yet effective changes, individuals can protect their knees and improve their quality of life.
Regular Exercise
Engaging in low-impact exercises like swimming, cycling, or yoga maintains joint health and reduces stress on weight-bearing joints. These activities help improve range of motion, build endurance, and enhance overall joint flexibility. Regular exercise also promotes circulation, delivering essential nutrients to the knee joint and supporting cartilage health.
Strengthening Core and Leg Muscles
Strengthening the quadriceps, hamstrings, and core provides better support, minimizing wear on the knee joint. Stronger muscles absorb shock more effectively, reducing the load on the joints during daily activities. Incorporating resistance training or bodyweight exercises into your routine can help maintain long-term knee stability.
Proper Footwear
Using shock-absorbing inserts or orthopedic shoes improves alignment and reduces knee strain. Proper footwear ensures even weight distribution, preventing undue stress on specific areas of the knee. It is particularly important for individuals with gait issues or those engaging in prolonged walking or standing.
Maintaining a Healthy Weight
Weight management decreases pressure on the joints, helping prevent cartilage loss and associated pain. Losing even a small amount of weight can significantly reduce stress on the knees, especially during activities like climbing stairs or walking. A balanced diet paired with regular physical activity supports healthy weight maintenance and overall joint health.
Relieve Bone-on-Bone Knee Pain with Austin Manual Therapy
Austin Manual Therapy offers specialized treatments designed to provide effective bone on bone knee pain relief. Techniques like joint mobilization, myofascial release, and manual therapy improve mobility, reduce joint swelling, and enhance synovial fluid circulation. Customized care plans emphasize non-invasive methods, including physical therapy and activity modifications, to optimize recovery.
Conclusion
Bone-on-bone knee pain is a challenging condition that requires proactive management. Understanding the symptoms, causes, and available treatment options can help individuals take the necessary steps to relieve pain, improve joint function, and enhance their overall quality of life. Incorporating non-invasive strategies like physical therapy, lifestyle adjustments, and targeted treatments can significantly reduce discomfort and delay the need for surgery. Early intervention, along with a commitment to maintaining joint health, plays a crucial role in managing this condition effectively.
FAQs
How to help bone-on-bone knee pain without surgery?
Non-invasive treatments like physical therapy, topical NSAIDs, hyaluronic acid injections, and acupuncture can help reduce inflammation and improve joint mobility. Combining these approaches with weight management and activity modifications can effectively relieve pain and delay the need for surgery.
What is the best support for a knee that is bone-on-bone?
Knee braces, orthotics, and assistive devices like canes or walkers provide stability and reduce discomfort. These supports help offload pressure from the affected joint, making movement more comfortable. Choosing the right support device based on the severity of the condition and activity level is essential for optimal relief and functionality.
Is it OK to walk with bone-on-bone knee pain?
Yes, walking is generally safe when done within your movement sweet spot, as it helps maintain joint mobility and strength. Stick to low-impact exercises and use supportive footwear to minimize joint stress. Listening to your body and avoiding overexertion ensures that walking remains a beneficial activity without exacerbating pain.





